What is the ethical impact that burnout has in Mental Healthcare staff?
Mental health care staff are at a high risk of experiencing burnout, this is a concern that needs to be addressed because it affects the employee and employer. Recognizing and addressing burnout in Mental health care staff should be an essential practice in a behavioral health organization. Jansee et al., 2018 stated that as to date, burnout remains a huge concern for mental health care organizations, since the negative impact associated with burnout affects staff, patients, families and the organizations.
Did you know that burnout is highly underscored and often untreated! On an organization level, literature states how problematic burnout can be. It was reported that employees who experience burnout have increased absenteeism, tardiness, reduce job commitment, poor job performance and increased turnover rate. Burnout is linked to the high demand of cost-reduction, increased workload, being short-staffed, increase patient acuity and complexity with no additional staff to support. In addition, staff who reported dissatisfaction with their jobs and who are considering leaving the organization are not putting as much effort into their work (Salyers et al., 2015).
Many may wonder what is burnout and am I experiencing?
Burnout is related to job dissatisfaction and it also is seen as damaging the morale of other employees, which in turn leads to increased staff turnover rates. Burnout is defined as a psychological syndrome related to excessive response to chronic stressors on the job. There are three key factors that are corelated as response to burnout; feeling of cynicism and detachment from the job, overwhelming exhaustion and a sense of ineffectiveness and lack of accomplishment (Janssen et al., 2018).
A study completed by Dreison et al., 2018, reports that high levels of burnout increased the risk of absence related to mental and behavioral disorders, as well as diseases of the circulatory, respiratory, and musculoskeletal systems. In mental health, staff absences and turnover are correlated with reduced fidelity to evidence-based practices and increase the costs of recruiting and training new staff.
How does policy decision making relate to burnout seen in employees?
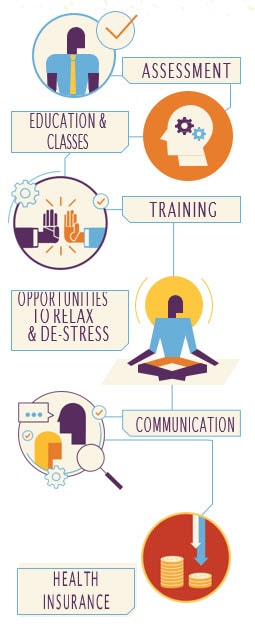
The Commission on Health and Safety and Workers’ Compensation works closely with organization in assisting in developing and implementing policies for their organization and employees. Workplace wellness/health promotion has been defined as the combined efforts of employers and employees to improve the health and well-being of individuals. Workplace wellness or health promotion programs are a combination of educational and organizational activities designed to support healthy lifestyles. These programs consist of health education, screening, and interventions designed to change workers’ behavior to achieve better health.
(AZFMC, 2019).
Programs that can be implemented at the workplace:
· Nutrition programs
· Smoking cessation programs
· Stress management programs
· Exercise and access to fitness and wellness centers
· Employee recognition
· Work and work-life balance initiatives
· Empowering employees
· Providing comfortable and quiet break rooms
(Wellness AZ, 2020)
What are some of the benefit of a healthy workforce?
We can all benefit from a healthy workforce, you may ask yourself how so? well employers see lower workers’ compensation insurance premiums; higher productivity and morale often result. And when workers are healthier, so are their families. This allows for organizations to be able to provide yearly raises, bonuses and decrease or maintain insurance premiums. A healthy workforce benefit EVERYONE!
Wellness programs should be designed to be flexible and respond strategically to situations as they arise. This, along with worker and management input, will help programs endure.
(Wellness AZ, 2020)
Governor Ducey talks about the Arizona Job Growth!
References:
AZFMC, 2019. Implementing wellness program. Retrieved from: https://www.azfmc.com/implementing-wellness-program
Dreison, K., Luther, L., Bonfils, K., Sliter, M., McGrew, J., Salyers, M., & Chen, Peter Y. (2018). Job Burnout in Mental Health Providers: A Meta-Analysis of 35 Years of Intervention Research. Journal of Occupational Health Psychology, 23(1), 18-30.
Janssen, M., Heerkens, Y., Kuijer, W., Van der Heijden, B., & Engels, J. (2018). Effects of Mindfulness-Based Stress Reduction on employees’ mental health: A systematic review. PLoS One, 13(1), E0191332.
Salyers, M., Fukui, P., Rollins, S., Firmin, A., Gearhart, L., Noll, R., . . . Davis, J. (2015). Burnout and Self-Reported Quality of Care in Community Mental Health. Administration and Policy in Mental Health and Mental Health Services Research, 42(1), 61-69.
Wellness AZ, 2020. Wellness AZ. Retrieved from: https://wellness.az.gov/hip